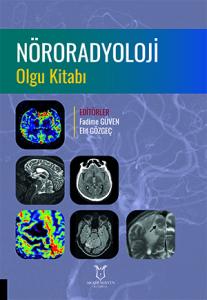
Vaka 19
Özet
Bu vaka, sistemik malignite öyküsü bulunan bir hastada gelişen beyin metastazını tanımlamaktadır. MRG’de çevresel kontrastlanan, geniş vazojenik ödemle çevrili kitle görünümü tipiktir. Difüzyon ve perfüzyon bulguları metastatik özellikleri destekler. Tedavi; cerrahi, radyocerrahi ve sistemik tedavilerin kombinasyonunu içerir.
Referanslar
Hakyemez B, Erdogan C, Gokalp G, et al. Solitary metastases and high-grade gliomas: radiological differentiation by morphometric analysis and perfusion-weighted MRI. Clinical Radiology. 2010;65(1):15-20. https://doi.org/10.1016/j.crad.2009.09.005
Wang S, Kim S, Chawla S, et al. Differentiation between glioblastomas and solitary brain metastases using diffusion tensor imaging. NeuroImage. 2009;44(3):653-660. https://doi.org/10.1016/j.neuroimage.2008.09.027
Law M, Cha S, Knopp EA, et al. High-grade gliomas and solitary metastases: differentiation by using perfusion and proton spectroscopic MR imaging. Radiology. 2002;222(3):715-721. https://doi.org/10.1148/radiol.2223010558
Calli C, Kitis O, Yunten N, et al. Perfusion and diffusion MR imaging in enhancing malignant cerebral tumors. European Journal of Radiology. 2006;58(3):394-403. https://doi.org/10.1016/j.ejrad.2005.12.032
Hakyemez B, Erdogan C, Bolca N, et al. Evaluation of different cerebral mass lesions by perfusion-weighted MR imaging. Journal of Magnetic Resonance Imaging. 2006;24(4):817-824. https://doi.org/10.1002/jmri.20707
Bulakbasi N, Kocaoglu M, Ors F, et al. Combination of single-voxel proton MR spectroscopy and apparent diffusion coefficient calculation in the evaluation of common brain tumors. American Journal of Neuroradiology. 2003;24(2):225-233.
Cha S, Lupo JM, Chen MH, et al. Differentiation of glioblastoma multiforme and single brain metastasis by peak height and percentage of signal intensity recovery derived from dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging. American Journal of Neuroradiology. 2007;28(6):1078-1084. https://doi.org/10.3174/ajnr.A0484
Server A, Josefsen R, Kulle B, et al. Proton magnetic resonance spectroscopy in the distinction of high-grade cerebral gliomas from single metastatic brain tumors. Acta Radiologica. 2010;51(3):316-325. https://doi.org/10.3109/02841850903482901
Shibata S. Ultrastructure of capillary walls in human brain tumors. Acta Neuropathologica. 1989;78(6):561-571. https://doi.org/10.1007/bf00691283
Mangla R, Kolar B, Zhu T, et al. Percentage signal recovery derived from MR dynamic susceptibility contrast imaging is useful to differentiate common enhancing malignant lesions of the brain. American Journal of Neuroradiology. 2011;32(6):1004-1010. https://doi.org/10.3174/ajnr.A2441
Desbarats LN, Herlidou S, De Marco G, et al. Differential MRI diagnosis between brain abscesses and necrotic or cystic brain tumors using the apparent diffusion coefficient and normalized diffusion-weighted images. Magnetic Resonance Imaging. 2003;21(6):645-650. https://doi.org/10.1016/s0730-725x(03)00084-5
Hartmann M, Jansen O, Heiland S, Sommer C, Münkel K, Sartor K. Restricted diffusion within ring enhancement is not pathognomonic for brain abscess. American Journal of Neuroradiology. 2001;22(9):1738-1742.
Kim DS, Na DG, Kim KH, et al. Distinguishing tumefactive demyelinating lesions from glioma or central nervous system lymphoma: added value of unenhanced CT compared with conventional contrast-enhanced MR imaging. Radiology. 2009;251(2):467-475. https://doi.org/10.1148/radiol.2512072071
Demir MK, Kılıç D, Zorlu E, et al. Giant intracranial cavernous malformations: a review on magnetic resonance imaging characteristics. Indian Journal of Radiology and Imaging. 2024;34(4):511-520. https://doi.org/10.1055/s-0044-1779587
Lyndon D, Lansley JA, Evanson J, et al. Dural masses: meningiomas and their mimics. Insights into Imaging. 2019;10(1):11. https://doi.org/10.1186/s13244-019-0697-7
Kamiryo T, Lopes MBS, Kassell NF, et al. Radiosurgery-induced microvascular alterations precede necrosis of the brain neuropil. Neurosurgery. 2001;49(2):409-415. https://doi.org/10.1097/00006123-200108000-00026
Long DM. Capillary ultrastructure in human metastatic brain tumors. Journal of Neurosurgery. 1979;51(1):53-58. https://doi.org/10.3171/jns.1979.51.1.0053
Mitsuya K, Nakasu Y, Horiguchi S, et al. Perfusion-weighted magnetic resonance imaging to distinguish the recurrence of metastatic brain tumors from radiation necrosis after stereotactic radiosurgery. Journal of Neuro-Oncology. 2010;99(1):81-88. https://doi.org/10.1007/s11060-009-0106-z
McDermott S, Barajas RF, Cha S, et al. Distinguishing recurrent intra-axial metastatic tumor from radiation necrosis following Gamma Knife radiosurgery using dynamic susceptibility-weighted contrast-enhanced perfusion MR imaging. American Journal of Neuroradiology. 2009;30(2):367-372. https://doi.org/10.3174/ajnr.A1362
Kimura T, Sako K, Tanaka K, et al. Evaluation of the response of metastatic brain tumors to stereotactic radiosurgery by proton magnetic resonance spectroscopy, 201TlCl single-photon emission computerized tomography, and gadolinium-enhanced magnetic resonance imaging. Journal of Neurosurgery. 2004;100(5):835-841. https://doi.org/10.3171/jns.2004.100.5.0835
Schlemmer HP, Bachert P, Herfarth KK, et al. Proton MR spectroscopic evaluation of suspicious brain lesions after stereotactic radiotherapy. American Journal of Neuroradiology. 2001;22(7):1316-1324.
Soffietti R, Cornu P, Delattre JY, et al. EFNS guidelines on diagnosis and treatment of brain metastases: report of an EFNS task force. European Journal of Neurology. 2006;13(7):674-681. https://doi.org/10.1111/j.1468-1331.2006.01506.x
Barnholtz-Sloan JS, Sloan AE, Davis FG, et al. Incidence proportions of brain metastases in patients diagnosed (1973 to 2001) in the Metropolitan Detroit Cancer Surveillance System. Journal of Clinical Oncology. 2004;22(14):2865-2872. https://doi.org/10.1200/jco.2004.12.149
Schiff D. Single brain metastasis. Current Treatment Options in Neurology. 2001;3(1):89-99. https://doi.org/10.1007/s11940-001-0027-4
Kralik SF, Kamer AP, Ho CY. Diagnostic imaging of intracranial metastasis. Current Problems in Cancer. 2015;39(3):99-112. https://doi.org/10.1016/j.currproblcancer.2015.03.003
Ercan N, Gultekin S, Celik H, et al. Diagnostic value of contrast-enhanced fluid-attenuated inversion recovery MR imaging of intracranial metastases. American Journal of Neuroradiology. 2004;25(5):761-767.
Schellinger PD, Meinck HM, Thron A. Diagnostic accuracy of MRI compared to CCT in patients with brain metastases. Journal of Neuro-Oncology. 1999;44(3):275-281. https://doi.org/10.1023/a:1006308808769
Baleriaux D, Colosimo C, Ruscalleda J, et al. Magnetic resonance imaging of metastatic disease to the brain with gadobenate dimeglumine. Neuroradiology. 2002;44(3):191-203. https://doi.org/10.1007/s002340100636
Runge VM, Kirsch JE, Burke VJ, et al. High-dose gadoteridol in MR imaging of intracranial neoplasms. Journal of Magnetic Resonance Imaging. 1992;2(1):9-18. https://doi.org/10.1002/jmri.1880020103